Delta-9-tetrahydrocannabinol, or THC, is the key psychoactive THC compound in cannabis. It’s responsible for the ‘high’ from marijuana and is essential in both recreational and medical contexts. This article will explore THC’s benefits, risks, and uses..
What is THC?
Delta-9-tetrahydrocannabinol, commonly known as THC, is the principal psychoactive component of the cannabis sativa plant. This compound is primarily responsible for the euphoric “high” that users experience when consuming marijuana. THC’s psychoactive properties are what set it apart from other cannabinoids found in the cannabis plant, making it a focal point in both recreational and medical marijuana use.
THC was first isolated in 1964 by Israeli chemist Raphael Mechoulam, forever changing our understanding of the cannabis plant. Its molecular formula, C21H30O2, reveals the intricate structure that underpins its powerful effects. The primary form of THC in cannabis plants is tetrahydrocannabinolic acid (THCA), which converts to THC through a process called decarboxylation, triggered by heat.
The resin produced by the glands of cannabis plants, particularly around the flowering tops, is the primary source of THC. This resin contains the highest concentration of THC, making it a key component in various cannabis products such as hash oil and cannabis extracts. The psychoactive effects of THC are well-documented, influencing mood, perception, and cognition, which are central to its recreational use and therapeutic applications.
Understanding THC within the broader spectrum of cannabis compounds highlights both its psychoactive effects and medical potential. Ongoing research continues to reveal the multifaceted applications of this powerful compound.
Mechanism of Action
THC exerts its effects by interacting with the body’s endocannabinoid system, specifically targeting cannabinoid receptors. As a partial agonist at the CB1 receptor, THC influences its psychoactive properties, which are predominantly experienced in the central nervous system. This interaction is what produces the well-known psychoactive effects of cannabis, such as altered mood, perception, and cognitive function.
The binding of THC to CB1 receptors modulates the release of various neurotransmitters, impacting both inhibitory and excitatory signals. This modulation can lead to alterations in pain perception and appetite regulation, making THC a valuable compound in managing symptoms like chronic pain and lack of appetite. The activation of CB1 receptors also plays a role in the suppression of pain responses through central mechanisms.
THC’s high lipid solubility means it can easily cross the blood-brain barrier, leading to its rapid onset of effects when inhaled. This property also contributes to its prolonged presence in the body when consumed orally, affecting its overall impact on the central nervous system. The interaction of THC with the brain’s reward pathways can enhance feelings of euphoria and increase appetite, which are beneficial in medical contexts like cancer and AIDS treatment.
Ongoing research is delving deeper into how THC interacts with the endocannabinoid system to regulate various physiological processes. These studies aim to better understand its therapeutic potential, particularly in managing mood disorders, pain, and other health conditions. Uncovering more about THC’s mechanism of action expands its role in both medical and recreational settings.
Medical Applications of THC
The medical applications of THC are as diverse as they are promising. Recognized for its effectiveness in managing nausea and stimulating appetite in patients undergoing chemotherapy, THC has carved out a significant niche in medical treatments. Its psychoactive properties, while often associated with recreational use, also play a crucial role in its therapeutic potential.
THC’s approved uses and potential therapeutic applications profoundly impact medical cannabis. The specific conditions for which THC is currently approved and emerging areas of research highlight its broader potential.
Approved Uses
The FDA has authorized the use of dronabinol, a synthetic form of THC, for treating AIDS-related anorexia and chemotherapy-induced nausea. This approval underscores the compound’s effectiveness in managing severe symptoms that are often resistant to other treatments. Dronabinol is specifically approved for these conditions due to its ability to stimulate appetite and reduce nausea, providing much-needed relief to patients.
Another synthetic THC compound, nabilone, is also approved for chemotherapy-induced nausea. Both dronabinol and nabilone have demonstrated significant effectiveness as antiemetics, helping patients manage the debilitating side effects of cancer treatment. These synthetic cannabinoids offer a controlled and reliable way to harness the benefits of THC for medical purposes.
These compounds’ approval marks a significant advance in THC’s medical use. By providing effective relief for specific conditions, dronabinol and nabilone underscore THC’s therapeutic potential and pave the way for further research and development.
Potential Therapeutic Uses
Beyond its approved uses, THC exhibits a range of pharmacological effects that suggest broader therapeutic potential. Its analgesic and anti-inflammatory properties make it a promising candidate for treating chronic neuropathic pain and other pain-related conditions. Cannabinoid receptors play a key role in the pathways that regulate analgesia, highlighting the importance of THC in managing pain.
Studies have indicated that synthetic THC can alleviate symptoms of fibromyalgia and chronic neuropathic pain, offering a potential alternative to traditional pain medications. Preliminary research also suggests that THC may inhibit the growth of certain cancer cells, including breast cancer, pointing to its potential role in cancer treatment.
Investigations into THC’s effectiveness in managing pain, inflammation, and chronic diseases suggest its potential as an alternative therapy. Researchers are also exploring optimal THC and CBD ratios to maximize benefits while minimizing adverse effects.
Emerging research on THC’s impact on the gut microbiome underscores its potential in treating various health conditions. Continued scientific exploration will likely expand THC’s role in medical cannabis. The therapeutic potential of this compound, coupled with ongoing clinical trials, may lead to new and innovative treatments for a range of conditions.
Administration Methods
THC can be administered through various methods, each with its own set of benefits and challenges. Oral administration, such as through capsules, edibles, and tinctures, offers a discreet and controlled way to consume THC. However, oral THC formulations exhibit significant variability in how quickly and efficiently they are absorbed into the bloodstream, leading to inconsistent effects.
Inhalation methods, such as smoking cannabis cigarettes and vaporization, provide a more immediate onset of effects. Smoking cannabis typically leads to the onset of psychoactive effects within a minute. Vaporization, on the other hand, avoids many harmful byproducts associated with smoking, making it a more health-conscious method of consumption. These methods are often preferred for their rapid effects and ease of use.
Edibles have become a popular form of cannabis consumption, offering a convenient and tasty way to ingest THC. However, the delayed onset of effects with edibles can result in accidental overconsumption, as users may ingest more THC than intended while waiting for the effects to kick in. Recognizing the nuances of each administration method ensures safe and effective THC use.
Adverse Effects
While THC offers numerous benefits, it is not without its risks. Cannabis products containing THC can induce significant alterations in mood, thinking, and perception of reality. High levels of THC can lead to serious health risks, particularly to the brain and other bodily systems. Commonly reported adverse effects include dysphoria, hallucinations, paranoia, sedation, confusion, headache, dry mouth, euphoria, and hypotension.
High doses of THC can result in serious side effects, including dependence, severe nausea, vomiting, and breathing problems. One specific condition associated with heavy THC use is cannabinoid hyperemesis syndrome (CHS), characterized by severe nausea and vomiting that does not respond to typical anti-nausea medications. THC poisoning can also occur, leading to symptoms such as extreme confusion, paranoia, elevated heart rate, and severe nausea.
Higher doses of THC are particularly associated with psychiatric symptoms, including hallucinations, delusions, and paranoia. Unintentional injuries, such as accidents, may result from impaired judgment caused by THC toxicity. Moreover, THC use can trigger relapse in schizophrenia and is linked to other psychiatric conditions such as psychosis, depression, anxiety, and substance use disorders.
The cardiovascular effects of THC, such as tachycardia (elevated heart rate), bradycardia (slowed heart rate), and orthostatic hypotension, further underscore the need for caution. Recognizing these adverse effects is crucial for anyone considering THC use, whether medically or recreationally.
Contraindications and Precautions
Certain populations should exercise caution when using THC. Pregnant women, for instance, are advised against using THC due to the potential risks to fertility and the unborn child. THC’s impact on fetal development can lead to long-term consequences, making it unsafe during pregnancy.
Patients with psychiatric conditions require careful monitoring, as THC can exacerbate symptoms of mania, depression, or schizophrenia. Individuals with a history of seizures should also use THC cautiously, as it may lower the seizure threshold and potentially trigger seizures. Older adults, who may be more sensitive to THC, should start at the low end of the dosing range and be monitored closely for any adverse effects.
The importance of dosing and monitoring cannot be overstated. Those with a history of drug abuse face an increased risk of dependence, further highlighting the need for careful consideration and professional guidance when using THC. These precautions can mitigate risks associated with THC use.
THC Toxicity and Overdose Risks
Recognizing THC toxicity and overdose risks is crucial for safe consumption. The potentially lethal human dose of THC ranges from 4 to 15 grams, although such doses are rarely, if ever, encountered in typical use. The median lethal dose (LD50) of THC for female rats when administered orally is 730 mg/kg, illustrating the variability of toxicity across species.
Overdose effects associated with high doses of THC include rising emergency room visits for edibles, although no deaths have been reported. The prolonged effects and high potency of edibles pose significant overdose risks, particularly for inexperienced users. Serious side effects are linked with consuming 50 mg or more of THC, highlighting the importance of understanding dosage and individual tolerance.
Children are particularly vulnerable to THC poisoning due to their smaller size and weight. Proper storage of THC products is essential to prevent accidental ingestions, especially among children.
In cases of THC overdose, supportive care and symptom management are the primary approaches, with gut decontamination being a common first aid step for oral ingestion. Monitoring for respiratory insufficiency is critical in patients experiencing THC toxicity. Recognizing these risks and taking precautions can prevent adverse outcomes associated with THC use.
THC in Medical Cannabis vs. Recreational Use
THC’s role in medical cannabis and recreational use presents a fascinating dichotomy. While it is commonly used as a recreational drug, making cannabis the most used illicit substance globally, its medical applications are equally significant. Medical marijuana use has a history spanning over 3,000 years, typically requiring a qualifying condition for legal use, which varies by state.
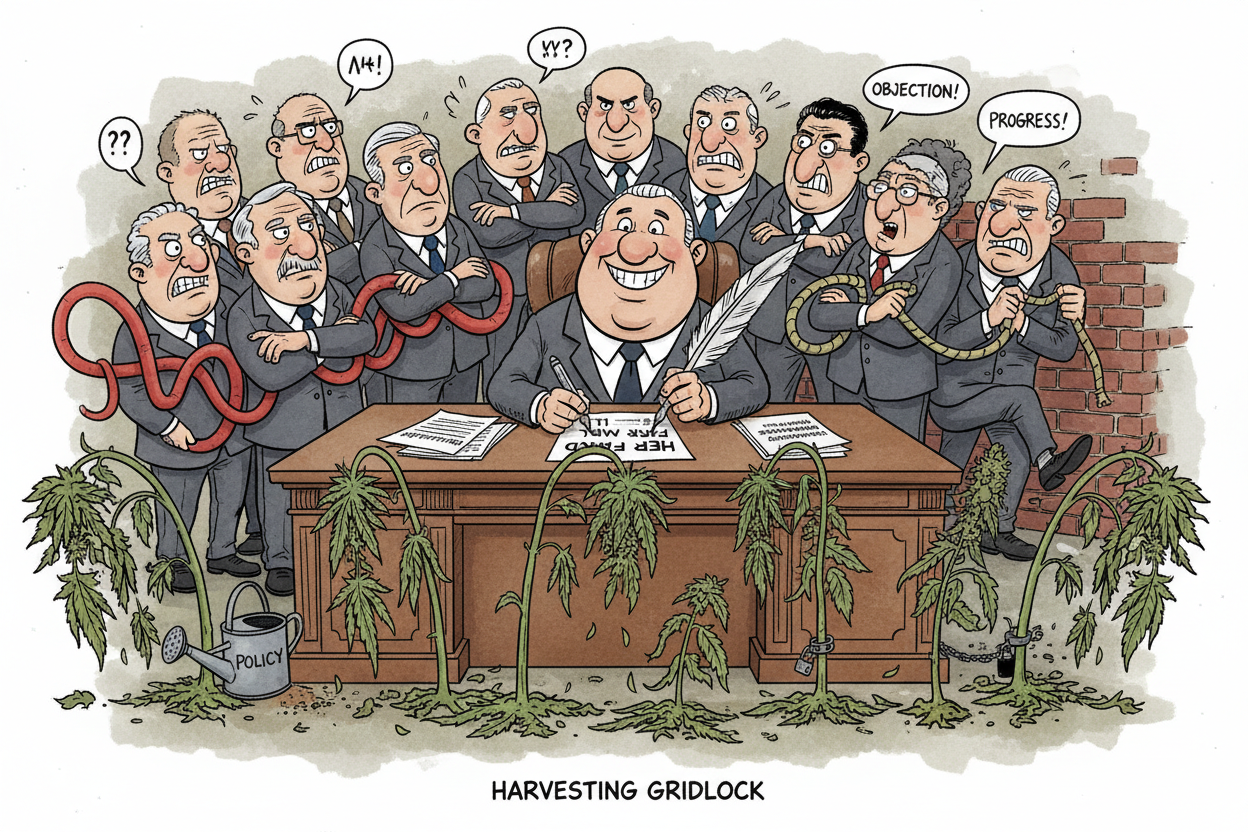
In the United States, THC is classified as a Schedule I controlled substance under federal law, making it illegal. However, over half of the states have legalized medicinal marijuana, reflecting a growing recognition of its therapeutic potential. The THC concentration in cannabis products can vary widely, from as low as 1% to as high as 80%, affecting both the intensity and duration of its effects.
Recognizing the differences between Hemp and Marijuana derived THC is crucial. Medical cannabis is often prescribed for specific conditions, with carefully monitored dosages and administration methods designed to maximize therapeutic benefits while minimizing risks. In contrast, recreational use typically involves higher THC concentrations and less controlled consumption, which can increase the risk of adverse effects and substance use disorders.
The 2018 Farm Bill marked a significant milestone in the history of cannabis regulation in the United States, particularly with its implications for hemp. By redefining hemp to include any part of the cannabis plant with a THC concentration of no more than 0.3% on a dry weight basis, the bill federally legalized the cultivation, production, and sale of hemp and its derivatives. This pivotal legislation not only opened doors for agricultural and commercial opportunities but also distinguished hemp from marijuana under federal law, thus removing it from the Controlled Substances Act. Consequently, this has led to an explosion in the popularity of CBD products derived from hemp, hailed for their potential health benefits without psychoactive effects. The 2018 Farm Bill represents a turning point in how hemp is perceived and utilized in America, promising significant economic impact and fostering new research into its myriad uses and benefits.
Ongoing Research and Future Directions
Current research emphasizes THC’s therapeutic potential for various health conditions, particularly chronic pain and appetite stimulation. Studies explore THC’s safety, dosage, and long-term impacts, considering its psychoactive effects and potential adverse outcomes. Randomized clinical trials and quantitative systematic reviews are crucial for establishing evidence-based guidelines for THC use. The National Institute of Health and other research bodies are funding ongoing studies to investigate the full spectrum of THC’s medical applications. These trials aim to provide a clearer understanding of how THC can be safely and effectively integrated into medical treatments.
Future THC research will explore its impact on the gut microbiome, potentially enhancing its therapeutic efficacy for various disorders. Additionally, researchers are investigating the optimal ratios of THC to CBD to maximize benefits while minimizing adverse effects. Such studies are essential for developing new and innovative treatments that harness the full potential of THC.
As new insights into THC emerge, its role in medicine is likely to expand. The ongoing research and future directions in this field hold promise for improved treatments and a better understanding of this powerful compound.
Summary
The journey through the world of THC reveals a compound with significant therapeutic potential and notable risks. From its role as the main psychoactive component of the cannabis sativa plant to its diverse medical applications, THC stands out as a critical player in both medical and recreational contexts. Understanding its mechanism of action, approved uses, and potential therapeutic benefits provides a comprehensive view of its capabilities.
However, the adverse effects and risks associated with THC use cannot be overlooked. Careful monitoring, appropriate dosing, and adherence to safety measures are essential for minimizing these risks. The differences between medical and recreational use further underscore the need for controlled and informed consumption of THC.
As ongoing research continues to explore the therapeutic potential of THC, the future holds promise for new treatments and a deeper understanding of this complex compound. By staying informed and cautious, users can harness the benefits of THC while mitigating its risks, paving the way for innovative medical applications and safer recreational use.
Frequently Asked Questions
What is THC and where does it come from?
delta-9-tetrahydrocannabinol, is the primary psychoactive compound derived from the resin of the cannabis sativa plant's flowers. It was first isolated in 1964, marking a significant development in cannabis research.
How does THC affect the body?
THC significantly impacts the body by interacting with the endocannabinoid system, specifically targeting CB1 receptors. This interaction alters mood, pain perception, appetite, and cognitive functions.
What are the approved medical uses of THC?
THC is approved for medical use in treating chemotherapy-induced nausea and AIDS-related anorexia, primarily through synthetic compounds such as dronabinol and nabilone. These medications are effective in stimulating appetite and alleviating nausea.
What are the potential risks of using THC?
Using THC carries potential risks such as mood alterations, hallucinations, and paranoia, particularly at high doses. Additionally, it may lead to dependence, exacerbate psychiatric conditions, and cause severe nausea or cardiovascular issues.
How is THC administered, and what are the differences between methods?
THC is administered via oral capsules, smoking, vaporization, and edibles, with inhalation methods providing rapid effects and oral methods offering delayed but prolonged effects, potentially increasing the risk of overconsumption. Understanding these differences is crucial for safe and effective use.




Share:
THC Candy for Travel: A Discreet, Convenient Companion
“Greenhouse vs. Indoor: Why Greenhouse THCa Flower Reigns Supreme”